[ad_1]
Scientists believe the fungus is not a threat to healthy people whose immune systems can fight it off. But it poses a danger to medically fragile people, including nursing home patients on ventilators and cancer patients on chemotherapy. Between 30 to 70 percent of hospitalized people who develop bloodstream infections are estimated to die.
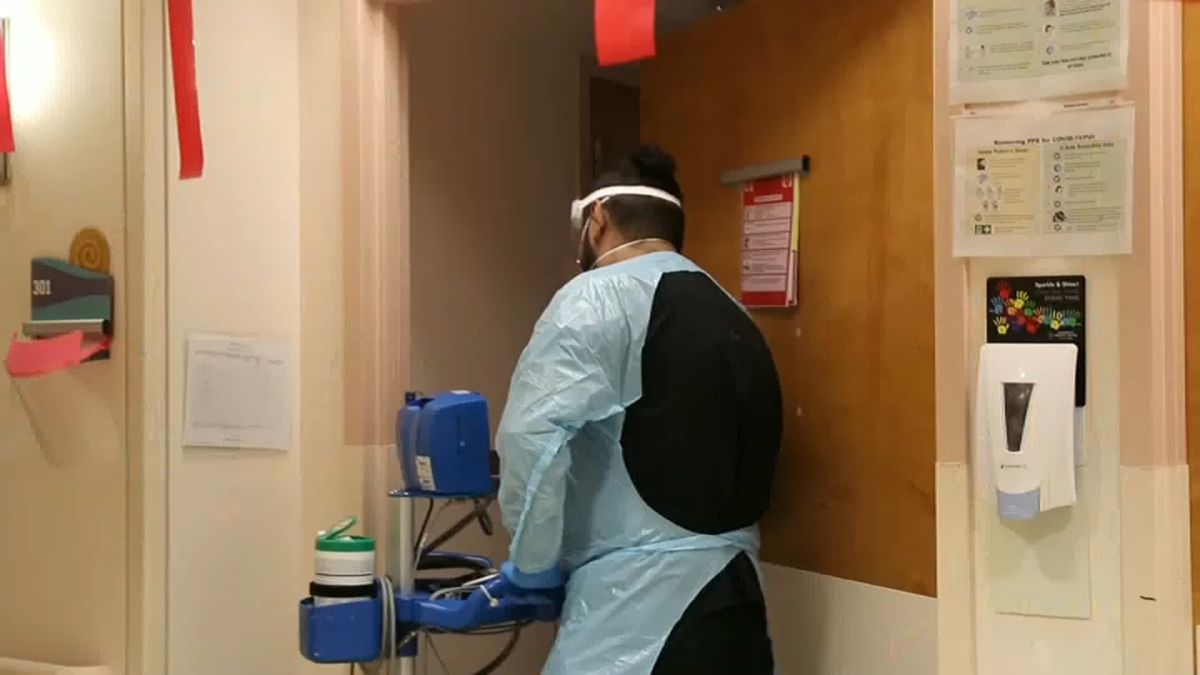
CDC experts say the increased spread underscores the need for robust infection control plans to reduce transmission of a fungus that can cause outbreaks because it lingers on surfaces and spreads through contact with patients and contaminated objects.
“If [the fungi] get into a hospital, they are very difficult to control and get out,” William Schaffner, a professor of medicine in the infectious diseases division of Vanderbilt University Medical Center. “They can persist, smoldering, causing infections for a considerable period of time despite the best efforts of the infection control team and everyone else in the hospital.”
Thorough cleaning of hospitals is challenging because of how long the fungus lingers on surfaces, said Meghan Lyman, a CDC medical officer and lead author of the paper detailing the fungus’s spread. Some disinfectants commonly used in health care settings don’t work against this fungus, she said.
The coronavirus pandemic exacerbated those challenges as health care workers scrambled with limited resources to contain the respiratory spread of that virus and to keep up with a flood of patients.
Authorities first detected Candida in the United States in 2016. The fungus is considered a serious global public health threat because it is resistant to different classes of antifungal drugs. Resistance to echinocandin drugs, often the first treatment deployed, remains rare in the United States, but researchers are concerned that a small but growing number of cases are resisting that class of drugs.
“There are a few antifungals in the pipeline, so that gives us some hope,” said Lyman.
The fungus has now been detected in more than half the states, with 17 states identifying their first case between 2019 and 2021. Most spread has occurred in long-term acute care hospitals and skilled-nursing facilities, where patients are more likely to be on ventilators, the CDC says. Case counts are likely an underestimate because screening requires specialized equipment and is conducted unevenly across the United States.
Candida can cause fatal infections in the bloodstream, heart and brain. The CDC does not track how many people died, and it can be difficult to discern cause of death when the patients at highest risk are often already fighting for their lives.
The emergence of the fungus, detected more than a decade ago in India, South Africa and South America, has perplexed researchers.
Fungi often cannot withstand the temperature of the human body, but one leading theory posits that Candida is now capable of doing so because it has evolved to survive in a warming world.
“This is how climate change or global warming can bring diseases because those in the environment have to adapt to survive and then have the capacity to survive in humans,” said Arturo Casadevall, a microbiologist at Johns Hopkins Bloomberg School of Public Health who has studied the fungus.
That has eerie parallels to the HBO drama “The Last of Us,” where the real-life cordyceps fungus that creates “zombie ants” adapts to a warming climate and infects humans, unleashing a zombie apocalypse.
Experts credit the show for generating interest in fungal infections that were often overshadowed by viruses and bacteria as the pathogens gripping public attention. Despite its deadly potential, the CDC says the spread of Candida can be stopped if hospitals emphasize surveillance, hand hygiene and deep cleaning with the proper disinfectants.
Lyman offered further reassurance: “We are glad to report it does not cause people to turn into zombies.”
[ad_2]
Source link