[ad_1]

zimmytws/iStock via Getty Images
Investment Thesis
Signed into law in 2010, the ACA has ushered in significant changes to how Americans receive health care. One area of focus was implementing a value-based approach to healthcare delivery away from volume-based fee-for-service payment models. Since then, the CMS (Centers for Medicare & Medicaid Services) has been experimenting with different models with different insurers, healthcare providers, and state government bodies. Danielle Cattel, an assistant professor at Erasmus University, studied 18 of these initiatives and found one commonality: a focus on Primary Care. This idea underpins the surge of the deal activity in the Primary Care market, manifested in Amazon’s (AMZN) acquisition of One Medical (ONEM), CVS’s (CVS) acquisition of Signify (SGFY), Walgreens (WBA) acquisition of Village MD and the wave of new managed care startups recently going public, including Clover Health (CLOV), and Alignment Healthcare (ALHC), both utilizing preventive care as a strategy to lower costs. The rationale behind the policy framework is simple: by investing in primary care, the healthcare system could reduce more expensive hospitalization.
This deal activity mirrors the size of the opportunity the CMS’s payment model transition offers. But the real question is, does agilon health (NYSE:AGL) provide such a chance? I don’t think so. The hottest asset in the healthcare market today is primary care facilities, and while AGL runs partnerships with 17 physician groups, spawning 2,200 primary care doctors, it doesn’t own the underlying assets, reducing its appeal as an M&A target, undermining its proposition compared to the likes of (AMED) and LifeStance Health (LFST), primary healthcare providers, who own the underlying assets, and derive the majority of earnings from Medicare and Medicaid programs.
One can’t find meaningful value when judging AGL’s business model on its merits. Running a hybrid breed of a re-insurance company and outsourcing business, it lacks a competitive edge, taking much risk for little return. The company has unlimited loss exposure for patients’ medical expenses, taking the risk from Humana (HUM) and UnitedHealth (UNH) for a fraction of profits under risk-sharing agreements, with PCPs earning most of the profits. AGL also provides outsourcing activities, maintaining the billing tasks on behalf of its providers.
Revenue Trends
Investors should be aware of several trends shaping the healthcare industry – especially for companies like AGL, which focuses its business on the Medicare market. These trends are driving changes across the entire healthcare system, including how providers deliver care and how they are paid for that care. However, despite the burden of healthcare expenditure on public budgets, I don’t believe that cutting these services is a politically viable option for elected officials or candidates running for office. In fact, the Healthy People 2030 initiative expanded national healthcare goals, as did the 2020 and 2010 initiatives before that.
AGL earns a capitated revenue per Medicare member covered. As it creates new partnerships, its revenue will increase, along with lives covered. Given its scope focusing on US seniors, its revenue comes from two sources 1) insurance companies offering Medicare Advantage and 2) the CMS under the Direct Contracting program. Thus, the company stands to benefit from demographic trends in the US as the baby boomer generation ages and become eligible for Medicare.
The most significant growth driver is intra-state and inter-state expansion through new provider partnerships. Currently, the company operates in seven states, up from five last year. Recently, it announced new partnerships in new states, including Maine, Minnesota, South Carolina, and Tennessee, adding nearly a quarter of a million lives to its platform starting in January 2023.
Two factors contribute to the company’s ability to sign in partnerships. First, leadership talent manifested in the ability to build and maintain partnerships with existing and new PCPs and payors (insurance companies). Steve Sell is the former CEO of Health Net, Centene’s (CNC) largest subsidiary. The board includes industry leaders with deep connections and expertise, such as Dr. Bill Wulf, the Chairman of America’s Physician Groups, a medical association with 300 institutional members. I believe that AGL’s management talent is critical to its success as the company continues to grow and expand beyond its current markets into additional states.
Second, the company offers PCPs and insurers an attractive deal, bearing most of the risk for a small fraction of profits. For example, it caps insurers’ exposure to the agreed capitated monthly payment per member. In contrast, its risk exposure to medical expenses is unlimited if the enrollees need additional care. Suppose its PCP partners succeed in lowering health expenses. In that case, it only shares a fraction of profits while maintaining managerial tasks such as collection, billing, liquidity support, squeezing margins, and underpinning our hold rating.
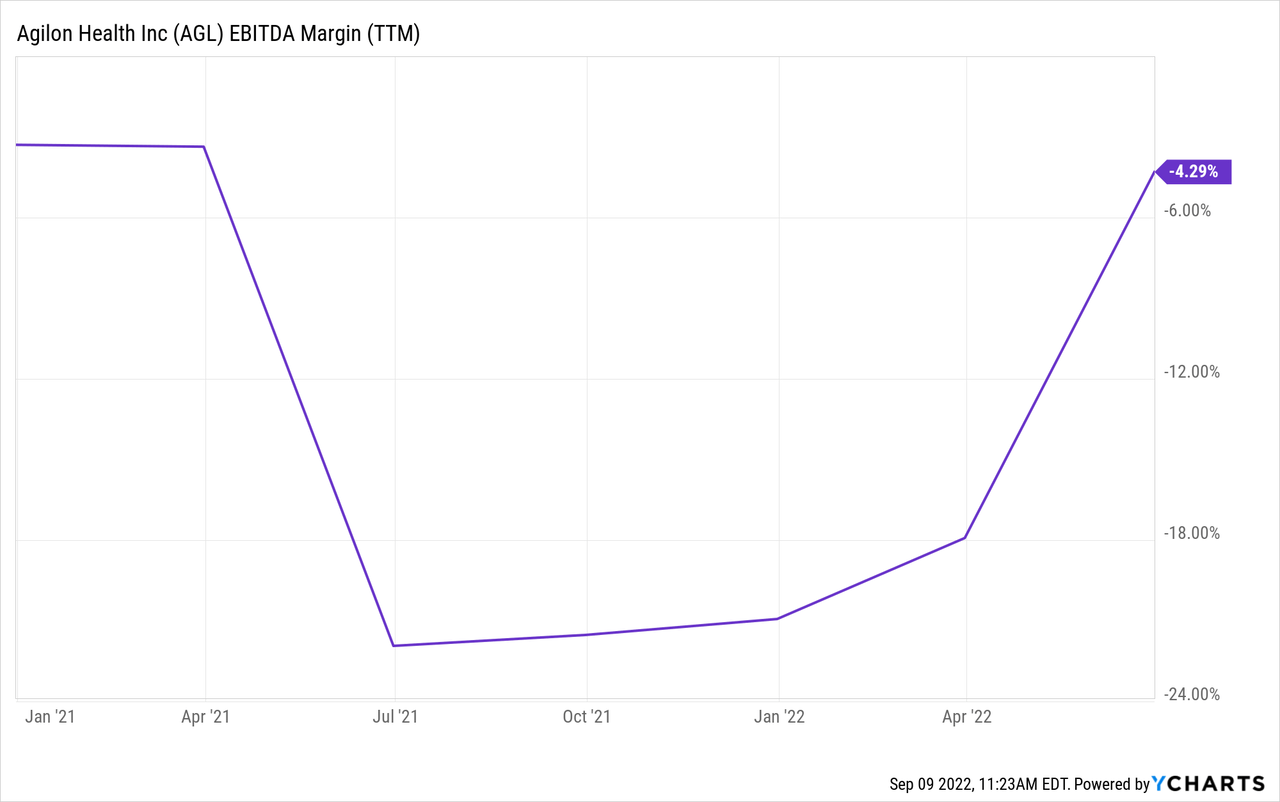
Margin Trends
There is no doubt in my mind that AGL can generate growth for the reasons stated above. However, there is still a question about valuation. The company’s business model is unique, capitalizing on CMS’s value-based care initiatives to lower healthcare spending. However, it lacks a competitive edge. Many insurance companies operate similar risk-sharing programs directly with their providers’ networks. Moreover, the absence of the economics of scale limits revenue growth benefits. The variable costs per enrollee are high.
Finally, one can’t help but think that the insurance industry, including hybrid models such as AGL, is digging its grave. The Department of Housing and Human Services “HSS” sets the Medicare reimbursement rates based on average care expenditure (currently standing around $10,000 on average per enrollee per year.) The maximum gross margin allowed by insurance companies is 15% – 20% (depending on size). However, to encourage the adoption of value-based care practices, the CMS, under some programs, allows insurers to keep whatever savings they achieve beyond this gross margin range. Suppose the industry succeeds in changing standard procedures and lowering national average care expenditure. In that case, the HSS will likely respond by lowering its base reimbursement rates. That’s the whole point of these initiatives. Thus, I believe that, in some sense, AGL’s quest to expand margins is like pursuing a mirage, at least in the long run.
Summary
AGL’s prospects hinge on its ability to lower the cost of care for its members and keep them healthy (as indicated by the trend in healthcare utilization metrics). So far, so good. Margins have been improving, verifying the positive relationship between ACA-aligned care and cost reductions. One challenge, however, is maintaining positive margin momentum as it expands its PCP partnerships. Should it do so successfully, the company could hit a major milestone in its growth story. Still, execution risks are exacerbated by high variable costs, structurally low margins, and unlimited downside exposure to patients’ health care costs as a reinsurer of Medicare Advantage insurance participants. In the long run, margins will likely be capped by a dynamic base rate set by the HSS. For now, the price level is too high, given its challenges.
[ad_2]
Source link



