[ad_1]
In a moment where over 28% of Connecticut’s adults report symptoms of anxiety or depression —up from 19% just two years earlier— the country’s largest insurer is threatening to hinder access to much-needed mental health care.
The present ruling in the Wit v. United Behavioral Health (UBH) case emboldens insurers to cherry pick coverage for acute treatment rather than determining coverage based on the generally accepted standards of care, further denying individuals access to the long-term care that they need.
Our state and our nation are amid a dire mental health crisis, exacerbated further by the pandemic, which has driven individuals to seek care in record numbers. At Mental Health Connecticut (MHC), we advocate and educate Connecticut residents and their communities on the importance of mental health, connect individuals to support services, and resource communities with the tools they need to care for their loved ones.
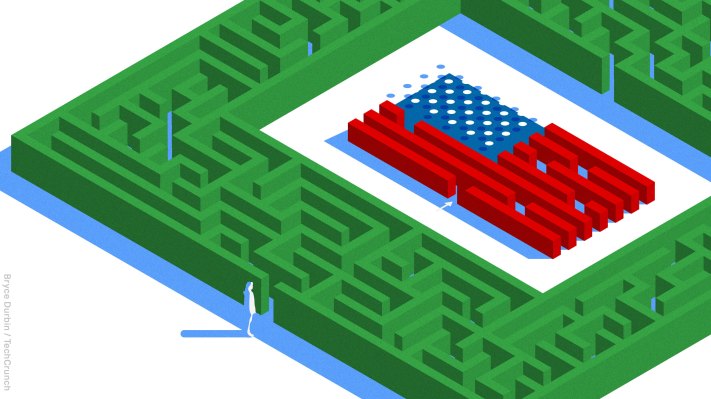
In our work, we frequently meet individuals who struggle to access the mental health care they need. We hear story after story of individuals who are denied care because their insurers determine medical necessity through their own standards, rather than evidence-based standards developed by medical professionals. This dynamic further inhibits access to mental healthcare within a system that is difficult to navigate for many other reasons.
A court ruling on March 5, 2019, found that United Behavioral Health, violated the 2008 Mental Health Parity and Addiction Equity Act (MHPAEA). This Federal Parity Law requires equal treatment by insurance companies of individuals who suffer from mental illnesses and addiction. However, in March of 2022, a three-judge panel at the 9th Circuit Court of Appeals reversed the District Court’s order with a seven-page ruling, arguing that it is “not unreasonable” for insurers to determine coverage inconsistently with generally accepted standards of care.
The disconnect between the robust and comprehensive 100-page plus District Court decision and the cursory 7-page reversal in Wit v. United Behavioral Health is unconscionable. The current ruling will embolden insurers to make decisions out of step with clinical standards. The ripple effects of this case will be felt not only in Connecticut – but nationwide.
As of May, Connecticut is one of four states (along with Rhode Island, Illinois, and California) who have filed amicus briefs urging for this reversal to be overturned. Leading the charge in Connecticut is Attorney General William Tong, who stated: “It makes no sense, when facing the worst public health crisis in America, for insurance companies to prioritize profits over people and to stand in the way of treatment and prevention.”
In March of this year, MHC joined 12 other Connecticut-based organizations in a letter supporting Attorney General Tong’s amicus brief. MHC and our allies are grateful for AG Tong’s support, and are eager to raise awareness regarding the devastating consequences of the present Wit ruling.
The present Wit ruling stands in contrast to the mission of Mental Health Connecticut and further complicates the work of our network of partners. Connecticut residents deserve consistent, reliable access to the care that they need in order to thrive and heal—and insurance coverage should be the last of their obstacles in seeking services to feel healthy and well.
The real-life implications of Wit v. UBH impacts far more than the 50,000 plaintiffs and thousands of Connecticut residents with mental health conditions. The present Wit ruling sets a nationwide precedent that insurers, rather than medical experts, can dictate what level of care should be covered for mental health patients.
We implore the Ninth Circuit Board of Appeals to defend patients’ right to access safe, consistent care, and grant en banc review of this case.
Luis Perez is President and CEO of Mental Health Connecticut.
[ad_2]
Source link