[ad_1]
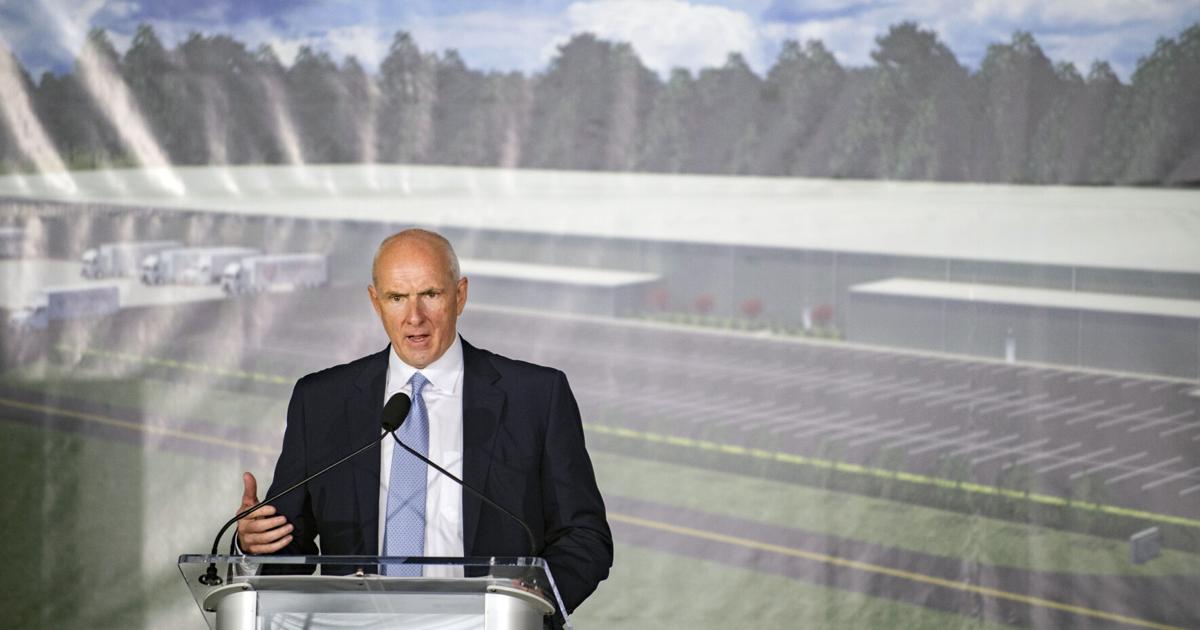
As Warner Thomas cracked open a Diet Coke in a chilly conference room the day after he announced he was leaving Ochsner Health, he was subdued and wistful when reflecting on his 24 years in New Orleans.
“It was a really hard decision … really hard,” he said, the executive’s typical assuredness missing from his voice. “I love New Orleans.”
He will be back, though. Warner is keeping his house in Uptown and plans to eventually retire in the city he’s called home since he became the chief operating officer of Ochsner at age 33. For now, the 56-year-old is renting in Sacramento, where he will run Sutter Health, California’s second-largest hospital system.
In the wake of his departure, Thomas leaves a legacy of unprecedented growth in Louisiana. Ochsner Health’s footprint swelled rapidly under his tenure, expanding from 8 hospitals and 38 clinics in 2012, when he became CEO, to 48 hospitals and over 300 clinics in ten years.
For some in Louisiana, Ochsner and Warner Thomas are synonymous, and the long-time executive is considered part of the system’s DNA. As his successor, Pete November, moves from chief financial officer to CEO on November 1, it’s unclear whether Ochsner will continue acquiring partnerships, affiliates and hospitals at a rapid clip. For now, November says he’s focused on the transition and the goals the hospital board already has in mind.
“The plan we have in place will remain in place,” he said. “Certainly, we’ll look at external growth opportunities, but our focus has got to be taking care of our patients and the communities we’re in today.”
Ochsner has grown ‘explosively’
Ochsner didn’t set out to be the biggest player in Louisiana or the Gulf South, Thomas said, but a few pivotal moves allowed it to gain a foothold in many communities. Along the way, the system developed a network of charter schools, built two manufacturing facilities for personal protective equipment, and ultimately became the largest private employer in the state.
“There’s only a couple of health systems in the country that have grown as explosively in this time period,” said Jeff Goldsmith, industry consultant and founder of Health Futures.
For his part, Thomas bristles at the idea that his drive is fueled by ambition for ambition’s sake. A comment from another system’s stakeholder – that Thomas wakes up every day and wants to “conquer the world” – is at odds with how he sees himself.
“They don’t know me,” he said, shaking his head. “People don’t think I’m sensitive, but I have a deep purpose in what we do every day.
“Are we fiscally responsible and make sure we operate our organization from a business perspective? Absolutely,” he continued. “But the reason we do it… is about patients and about our communities.”
Thomas acknowledges it has taken a relentless optimism to guide Ochsner from where it was when he joined as COO in 1998 to where it stands today.
“I think we do things very well,” said Thomas. “And if we do them well, why wouldn’t we try to impact more lives and take care of more people?”
A defining merger and Hurricane Katrina
Thomas identified two defining moments that allowed the system to expand. First, the Ochsner clinic and hospital merged into one non-profit foundation, known as the Ochsner Clinic Foundation, in 2001.
Prior to the merger, the for-profit clinic was owned by hundreds of physicians with 26 locations. The non-profit Alton Ochsner Medical Foundation included an educational and research arm, Ochsner Home Health, the Jefferson Highway campus and the Elmwood Fitness Centers. The move made the entity more powerful, cemented its non-profit status and centralized billing, resources and group purchasing power.
“That was really the defining event in the history of Ochsner to allow it to get to where it is today,” said Thomas.
The second moment was born out of the aftermath of Hurricane Katrina. As national chains retreated from waterlogged hospitals and the task of bringing skittish doctors and nurses back to the city, Ochsner swooped in.
“Katrina landed five or six other hospitals in their lap and then they took off from there,” said Walter Lane, a health care economist at the University of New Orleans. Lane is also a board member of Slidell Memorial Hospital, an Ochsner affiliate since 2016, but was not speaking on behalf of the hospital.
In an economist’s eyes, the trend of hospital consolidation was inevitable based on rising costs that have made it difficult for small shops to remain independent. But because Katrina made New Orleans a less desirable market, larger chains were uncertain about making a play for Louisiana’s market share. Thomas had an opportunistic vision of expansion when other systems were in retreat.
“What Warner saw was the trend happening nationally,” said Lane. “Warner had this vision, I think, recognizing if they didn’t do something, someone was going to.”
Ochsner Health’s first purchase after Katrina was three Tenet Hospital properties for $56.8 million, including the now infamous Memorial Hospital, where 45 patients died and controversy erupted over whether some stranded patients were euthanized.
“That was a huge bet at that time,” said Thomas, who described himself as a realist, but one that possesses an optimism that allows him to figure out most challenges.
“I think what we knew is that New Orleans was going to come back, but we didn’t know the timeframe,” he said. “We knew that the city couldn’t be successful if it didn’t have a great healthcare infrastructure.”
Thomas told the board that in two years they would probably be wondering why they bought the Tenet hospitals, and in five years they’d be glad they did.
Thomas made the first call to Tenet in late September, just weeks after Katrina while he was still living in his office on Ochsner’s main campus. Pete November was the lawyer on the other side of the Tenet deal.
November’s challenge
November spent much of his youth in Kentucky hospitals with his mother, a single parent who worked as both a home health and oncology nurse.
“I spent a lot of time with my mom in hospitals in the afternoon, waiting for my grandma to pick me up or waiting for my mom to get off her shift,” said November. “My mom only cared about one thing, and that was taking care of people.”
November has been at Ochsner for 10 years, recruited by Thomas after they negotiated the Tenet sale, and said he is now focused on the transition. Transitioning hospital systems can be notoriously difficult after long-time CEOs exit, industry experts said.
“A lot of times it’s really hard to follow,” said Goldsmith. “Often the charismatic CEO doesn’t do the hard work of building the next two layers of leadership so that someone is capable of stepping into his or her shoes, and continuing to rock and roll.”
Thomas said he feels OK leaving Ochsner now because the hospital, and its succession plan, are in a good place. For the past 20 years, he has identified who might succeed him in a yearly evaluation. When the Sutter offer came up, the board already had that list of names.
Nationally, many hospitals are in worse financial positions than they were a year ago because of rising costs. November’s challenge will be to align recent partners and affiliates with Ochsner’s way of doing things.
“When you grow that rapidly, you’ve really got a tremendous management issue on your hands,” said Chip Kahn, the President and CEO of the Federation of American Hospitals. “It takes many years to bring everybody into your culture.”
Louisiana is a particularly precarious market because of its poverty. Over 60% of births are paid for by Medicaid, Kahn pointed out. And although the population is sicker than the U.S. average, the diseases most often treated here – infections, multi-organ disease and severe cancer – don’t always provide hospitals with sufficient funding, especially if the patients are insured by Medicare or Medicaid.
“You have a lot of those patients in a place like Louisiana, with both the aging of the population and a poor population,” said Kahn.
Thomas said he was drawn to the California job because its reach is more significant.
“I feel like Ochsner is in a much better position today than when I came here in 1998,” said Thomas. “And it’s in a much better position today than it was when I took over as CEO in 2012. What excites me about Sutter is that I can have a broader impact and potentially help another organization reach its potential.”
Thomas did not say what he would be paid in his new role, but the Sutter CEO in 2019 made about $5.5 million in compensation, less than Thomas’ $6.8 million in 2020. But Sutter’s previous CEO, Patrick Fry, earned about $13.4 million in 2015.
[ad_2]
Source link