[ad_1]
Brain researchers have relied on devices called microelectrode arrays for decades, but the technology behind these devices has become increasingly outdated. Precision Neuroscience is developing a state-of-the-art alternative to implantation that is not only an order of magnitude larger, but also minimally invasive. With $41 million in new revenue raised by the bank, they are all about to enter the market complex.
To understand what is going on in the brain, sometimes an EEG or MRI is not enough from the outside – you have to go inside. For this purpose, implanted electrodes have been used for a long time, and arrays in formation are used to collect data from several points in the cortex at the same time.
But while an electrode array a dozen strong can be invaluable in a research setting, it’s simply insufficient as a functional brain-computer interface. The data density is too low for the patient to control the prosthesis or move the pointer on the screen. And you can’t just add more electrodes: because each one pierces the brain tissue and necessarily causes some damage, going from 100 arrays to 1,000 arrays causes 10 times the damage.
Precision Neuroscience aims to solve both problems with one major innovation: an ultra-thin electrode array that doesn’t need to pierce the brain at all, but can collect hundreds of times more data than traditional arrays.
Dr. Ben Rapoport, a neurosurgeon who spent decades working on the idea and founded the company in 2021, is a brainchild, so to speak.
“This was his life’s work,” says Precision CEO Michael Mager. “His view is that you always need a high density of electrodes, even for basic functions, and the technology should be deployed in a minimally invasive way, with no damage to the brain. Our hope is to balance tens of thousands of electrodes – and they cannot continue to penetrate the tissue from time to time.”
The array they create is called layer 7, the cortex itself has six layers, and the interface sits on top of it. A single layer 7 array is only slightly larger than a miniature, but has 1,024 microelectrodes on it, making it hundreds of times more dense than what’s commonly used today. And they’re designed to be used in their own array, basically spread across the brain region. Each array provides a fast and accurate picture of the activity of the cortical regions it covers.
These capabilities and details are impressive, but having the interface without craniotomy – open brain surgery – is perhaps even more important. Instead, the ultra-thin film-based layer 7 can be inserted into a small part of the skull – still brain surgery, to be sure, but a much less invasive method that doesn’t even require general anesthesia. It is attached to an external control unit, but the dimensions and specifications of that device vary according to different conditions.

Two cool Precision Neuroscience employees. You can see the installation on the microscope slide. Image Credits: Precision neuroscience
It is important to avoid the risks and complications of major surgery as the population that will benefit the most from such technology are people with existing neurological problems.
“There are tens of millions of people who suffer from stroke, TBI in the US alone. [traumatic brain injury]degenerative diseases… but for those patients there are no medical solutions we can offer beyond physical therapy,” Mager said.
“There are two broad use cases,” said chief product officer Craig Mermel. It is one of brain stimulation and two-way interface, but it is still a high test. We do this through ‘record and decode’, a research-backed approach to read data from people with epilepsy or stroke and translate impulses into motor or speech output.
This ability has been studied and demonstrated successfully in other contexts over the years, but the catch is that the implants themselves are “still in the research phase,” Mermel said. No one has put this into a clinical-grade system that patients can use. That [i.e. Layer 7] It does not harm the mind and becomes the most important aspect of our system. Every device has a lifetime, and you have to replace it; The fact that our interface is reversible and brain intact minimizes risk to the patient.
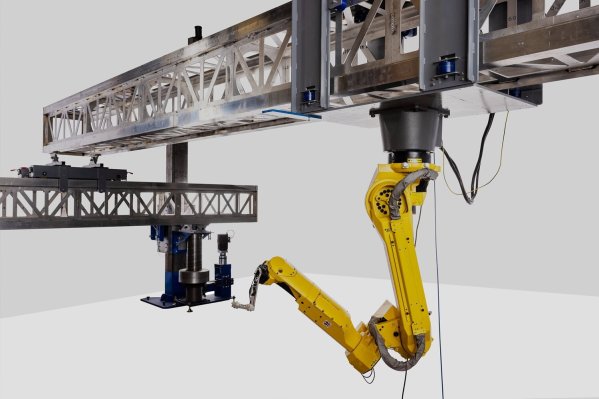
By now, most readers are wondering how this compares to Neuralink, the brain-computer interface company funded by Elon Musk. One important difference is that the Neuralink approach still involves a craniotomy and brain-piercing electrodes—although the ones now used and implanted robotically are much better and more sensitive. But Precision Neuroscience sees the company as a partner rather than a competitor.
“Really, what we’re talking about internally are different approaches that are appropriate for different situations,” Mager said. “It’s not going to be a one-size-fits-all market. There’s room for more than one company.
One of the challenges when developing any kind of medical device, to say nothing of a brain implant, is the monumental task of ensuring both applications and safety before going to market. And you can’t just build a widget – it needs to be distributed, supported, documented, etc.
“It’s not just the array, but the software – the complexity of machine learning is a must to drive a very powerful BCI. It’s a full-stack product that requires an interdisciplinary team to develop,” Mager said. “And so and then You must take it through the FDA inspection process.
Alongside this, the company is taking a two-pronged approach. At first they focus on short-term and emergency use, such as in a hospital setting – it can be life-saving when you understand what’s going on in the brain. They will submit their 510K application to the FDA along these lines later in the year and be ready to go when the agency gives the green light. Longer term, the plan is to secure a semi-permanent implant: the kind that a person can use all day every day for a year from home or on the go. That’s a different risk profile and a more rigorous approval process.

Precision’s Stephanie Galabi examines the Layer 7 implant. Image Credits: Precision neuroscience
Such relatively long-term considerations are common in medicine, but less so in venture-backed startups. Why ask VCs when they’re interested in faster and easier-to-scale companies like software and services?
“It was a big mistake, we should have started a software company. I talk to Craig about this all the time! ” Mager joked. But of course, despite the challenges and times, there is a not easy group of VC companies that are excited to invest in companies that want to have a big impact on human health and build a big company – not in two-three years, but 10 years.
Here, Mager credits Musk with helping to popularize the idea that Mager can support larger, long-term endeavors like SpaceX and Tesla, not just quick-scale software companies that sell within a year or two. A rocket company might not have seemed like much of an effort to fund with venture capital 10 or 15 years ago, but no one is asking for it now. The same may be true for neural networks — “and until then we can create some meaningful clinical good.”
The $41 million B round will allow Precision to continue working toward FDA approval and further develop and support the Layer 7 stack, from hardware to training and customer service. The round was led by Forepont Capital Partners. Mubadala Capital, Draper Associates, Alumni Ventures, re.Mind Capital, Steadview Capital and B Capital Group
[ad_2]
Source link