[ad_1]
But after Health and Human Services officials announced their proposal on Aug. 4, Paul Chaplin, chief executive of Bavarian Nordic, the vaccine’s manufacturer, called a senior U.S. health official and accused the Biden administration of breaching its contracts with his company by planning to use the doses in an unapproved manner. Even worse, said two people with knowledge of the episode, Chaplin threatened to cancel all future vaccine orders from the United States, throwing into doubt the administration’s entire monkeypox strategy.
“People are begging for monkeypox vaccines, and we’ve just pissed off the one manufacturer,” said one official who spoke on the condition of anonymity because they were not authorized to comment.
The behind-the-scenes clash with Bavarian Nordic, which has not previously been reported, was just the latest episode in a monkeypox response beset by turf wars, ongoing surprises and muddled messaging, with key partners frequently finding themselves out of sync as they race to catch up to a rapidly unfolding crisis.
For two months, the Biden administration has been chased by headlines about its failure to order enough vaccines, speed treatments and make tests available to head off an outbreak that has grown from one case in Massachusetts on May 17 to more than 13,500 this week, overwhelmingly among gay and bisexual men. And 100 days after the outbreak was first detected in Europe, no country has more cases than the United States — with public health experts warning the virus is on the verge of becoming permanently entrenched here.
“I think there’s a potential to get this back in the box, but it’s going to be very difficult at this point,” Scott Gottlieb, who led the Food and Drug Administration under President Donald Trump and has advised the Biden administration on its response to public health outbreaks, said on CBS’s “Face the Nation” last week.
Interviews with more than 40 officials working on the monkeypox response, outside advisers, public health experts and patients show that despite efforts to learn from the nation’s coronavirus failures, officials struggled to meet growing demand for testing, vaccines and treatments. Early mistakes, including the failure to recognize the virus was spreading differently and far more aggressively than it had previously, and a plodding bureaucracy left hundreds of thousands of gay men facing the threat of an agonizing illness that has not led to U.S. fatalities but can cause painful lesions some have likened to being pierced by shards of glass while going to the bathroom. And experts fear broader circulation of a virus that can infect anyone by close contact.
Biden officials insist the nation’s response is at a turning point, touting a White House monkeypox team set up this month to lead the effort, the recent decision to declare monkeypox a public health emergency and the new vaccine plan to address growing demands for shots.
“The president asked me to come here and do this,” said Bob Fenton, the freshly installed national monkeypox coordinator, adding that his goal is to “control, contain, eliminate monkeypox here in the United States and to do that in accelerated fashion.”
The coming weeks will reveal whether the administration has overcome its early struggles — or whether too much time was lost as the virus took hold in the United States under a president who had vowed to prevent pandemics.
May 17: One confirmed U.S. infection
Demetre Daskalakis, a senior official at the Centers for Disease Control and Prevention, was working from home on HIV prevention projects over the May 14 weekend when CDC colleagues summoned him to an urgent call as cases of unusual lesions had begun to appear in Britain.
Daskalakis quickly brushed up on the symptoms and origins of monkeypox.
“I did the yeoman’s work of getting my infectious-disease biology textbook out and just reviewing stuff about monkeypox to be ready,” Daskalakis said. In subsequent days, Daskalakis and his colleagues would come to spend virtually all their time trying to understand the virus that appeared to be spreading rapidly among gay men who had not traveled to West or Central Africa, where monkeypox was historically confined.
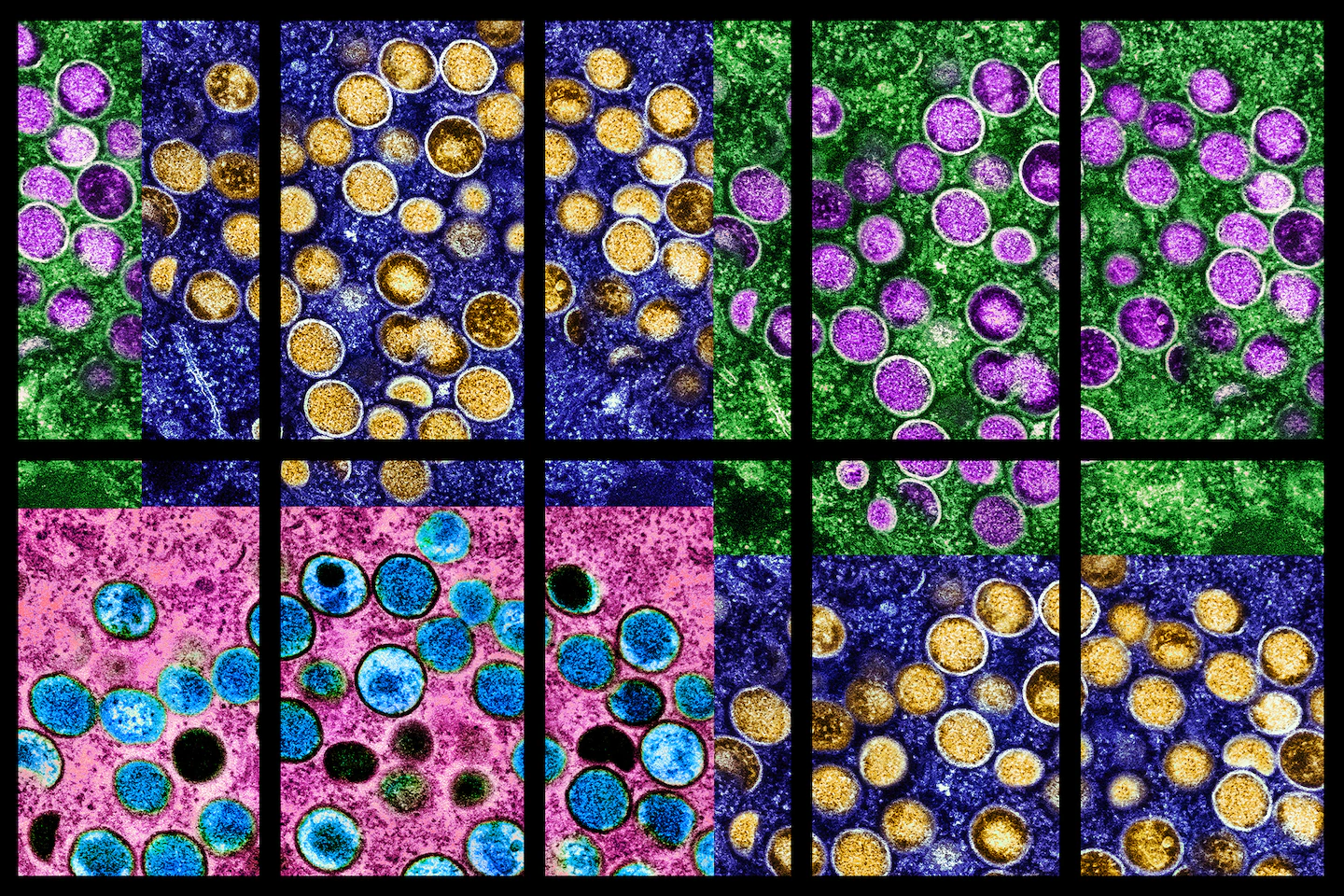
First discovered in laboratory monkeys in 1958, the virus, a cousin of the much deadlier smallpox, can result in severe pain, lesions that scar and long-lasting complications, particularly in people with immune conditions.
In 2001, monkeypox was briefly on the radar of the nation’s health leaders, charged with building up a biosecurity apparatus following the Sept. 11, 2001, terrorist attacks. As then-HHS Secretary Tommy Thompson and other senior officials dined at Oceanaire, a seafood restaurant a few blocks from the White House, D.A. Henderson, godfather of the effort to eradicate smallpox, piped up about another threat to beware.
“Just wait another 20 years. Monkeypox in the Central African countries will make a major resurgence,” Henderson said, according to Michael Osterholm, a University of Minnesota infectious-disease expert who was at the dinner.
Some of those fears were realized in a 2003 U.S. monkeypox outbreak linked to pet prairie dogs, with 47 people in six states infected. But the episode passed with no deaths, and the virus was largely forgotten as other biological threats, including Ebola, challenged the Obama and Trump administrations.
So when Joe Biden campaigned for the presidency in 2020, it was the coronavirus — and not a quietly burbling monkeypox outbreak in Nigeria — that was top of mind as he repeatedly faulted Trump for dismantling a White House pandemic team that Biden said could have helped lead the global health fight. On his first day as president, Biden issued an executive order to restore the pandemic office as part of his National Security Council, saying its leader would be responsible “for monitoring current and emerging biological threats.”
By mid-May 2022 — as the first U.S. monkeypox cases were detected and experts feared that a new epidemic was underway — the task of coordinating the response largely had fallen to Raj Panjabi, a physician lionized for his work in global health, who led Biden’s pandemic office.
Panjabi believed that the United States had the tools and know-how to fight a virus thought to mostly spread by skin-to-skin contact that posed far fewer risks than the coronavirus.
“We have already worked to secure sufficient supply of effective treatments and vaccines to prevent those exposed from contracting monkeypox and treating people who’ve been affected,” Panjabi said on NPR on May 23, six days after the first U.S. monkeypox case was detected.
That reassuring message was amplified by other officials, including the president. “We have vaccines to care for it,” Biden said the same day at a news conference in Japan. “I think we do have enough to deal with the likelihood of the problem.”
But state officials were clamoring for more information on how to prioritize their response.
Anne Zink, chief medical officer for Alaska, recalled peering into her computer camera from her standing desk in her plant-filled home office just north of Anchorage for a Zoom call with CDC officials as state health officials pressed the agency for guidance on who should be prioritized for vaccinations.
“We need to move quickly. You know the data on this best. It would be very helpful to have clear direction from you all,” Zink said state officials insisted during the May 20 call.
Meanwhile, HHS officials were confronting a logistical problem: how to get enough vaccines to the United States, and how soon to do it.
At the time, the national emergency stockpile held 2,400 doses of Bavarian Nordic’s Jynneos, the only vaccine approved by the Food and Drug Administration for monkeypox. While the United States had purchased millions more potential doses, they sat in Bavarian Nordic’s factory in Denmark, either as finished doses in freezers or as raw materials, waiting to be turned into vaccines.
The U.S. stockpile also had hundreds of millions of shots of an older vaccine approved for the related smallpox virus, ACAM2000, although health officials were wary of using that vaccine — given the increased risk of side effects and even inadvertent illnesses — and considered it a fallback.
But the Jynneos doses in the stockpile were losing shelf life because its freezers were capable of storing the doses only at negative 20 degrees Celsius, while Bavarian Nordic’s freezers in Denmark kept doses stored at negative 50 degrees Celsius.
Shipping the doses would create additional challenges in keeping the vaccines as cold as possible for their 4,000-mile voyage to the United States.
“Every time we move doses from their freezer to the [stockpile] … we lose two years of shelf life,” said Dawn O’Connell, head of the Administration for Strategic Preparedness and Response, which oversees the national stockpile. “Every time we convert doses from [raw materials] to a vial, we lose seven years of shelf life.”
O’Connell and her deputies decided to order 36,000 vaccine doses May 20 after the first two cases of monkeypox were confirmed, and another 36,000 doses on May 27 — a step that some officials feared was an overreaction at the time but that would quickly feel insufficient as demand soared.
June 10: 59 confirmed U.S. infections
As cases climbed in June, White House officials continued to assure the public that the situation was being handled. Pride Month festivities celebrating gay life went on as planned around the country, many for the first time since the coronavirus pandemic began.
“We have tests for monkeypox, we have vaccines for monkeypox, and we have treatments for monkeypox,” Panjabi said in a news conference on June 10. “We have a multipronged approach to deploy those tools to ensure we’re fighting this outbreak as effectively as possible.”
But physicians, experts and patients described a different picture: growing delays in trying to access tests and treatments — and little visible urgency to fix it.
“The biggest mistake our advocates made, our community made early on in this outbreak was trusting Raj’s assurances,” said James Krellenstein, co-founder of PrEP4All, a group that advocates for access to HIV care. “That ultimately led to many of our community members being unnecessarily sick.”
As Panjabi’s team convened agency experts for multiple daily briefings, some leaders at the CDC began to fret that staff were spending so much time preparing for meetings that it was harder to focus on figuring out who was getting infected and how they were exposed. Outside experts said they had concerns that the White House pandemic office was too focused on narrow goals and metrics and not enough on setting a national strategy.
The White House declined to make Panjabi available for an interview. In response to questions about the administration’s handling of monkeypox, Adrienne Watson, National Security Council spokeswoman, defended the actions of top officials. “The NSC Global Health Security and Biodefense Directorate was in place to monitor and coordinate from day one of the outbreak,” she said in a statement.
Early on, every monkeypox test required physicians to first get permission from a city or state epidemiologist, often an hours-long process that required multiple phone calls or emails — before the sample was sent to a public health laboratory, which could take days to release results. Following CDC guidance, local officials also imposed strict requirements that tests could be administered only to patients with visible lesions — the telltale sign of monkeypox — or patients with rashes who had been potentially exposed. The CDC’s thinking was that testing the most at-risk people, followed by contact tracing, would give the United States the best shot at controlling the outbreak.
The restrictions created a chokehold: Only about a dozen tests per day were being performed nationwide in early June, at a time when officials believed hundreds or thousands of daily tests were needed to detect infection clusters and head off an outbreak.
The national response to the crisis felt like “paralysis by indecision,” said Lauren Sauer, director of the Special Pathogens Research Network within a government-funded consortium of medical centers focused on training and education, recalling the difficulty in identifying how many Jynneos doses were available in early June as she tried to plan her response.
At a June 9 meeting of pathogens researchers in a downtown D.C. hotel, Sauer learned about a monkeypox patient without visible sores who was tested only after an astute doctor swabbed a lesion near his anus. Sauer wondered, given the testing requirements at the time, how many others would be missed, and she texted two infectious-disease colleagues: “This is going to be another pandemic.”
Some health responders around the country, already worn down from two years of responding to the coronavirus, were grappling with how to prioritize a new viral threat yet to be linked to deaths. And communicating the risks of monkeypox to the public was proving to be a challenge, with officials struggling to warn the gay men who were disproportionately contracting the virus, often through sex with multiple partners, while not stigmatizing them.
By mid-June, D.C. health officials began recording cases transmitted between people with two degrees of separation.
On June 16, a man who participated in a porn shoot with dozens of people at a gay bathhouse in D.C. received a direct message on Twitter from a public health agency in Virginia, where he lived, that he had been exposed to the monkeypox virus.
He did not hear from the organizers of the shoot until nine days later, when he received an email that a “small number” of attendees had tested positive, according to a June 25 email shared with The Washington Post.
The man said he received a vaccination upon learning he had been exposed and did not develop symptoms. But at least four friends at the shoot fell ill within two weeks of filming, having yet to hear from contact tracers.
“Had they ordered the venue to notify attendees, we could’ve done a lot to mitigate local spread stemming from this event,” said the man, who spoke on the condition of anonymity for fear of repercussions at his day job.
In cities across the country, monkeypox patients were unable to provide the names or contact information of every sexual partner. And while health officials concluded the best way to slow the spread was to aggressively vaccinate high-risk groups — primarily sexually active gay and bisexual men — they had to fill out a time-consuming spreadsheet required by the CDC for every vaccine administered, said Patrick Ashley, a D.C. Department of Health official working on the monkeypox response.
Inside the Biden administration, officials such as White House covid coordinator Ashish Jha and infectious-disease expert Anthony S. Fauci had begun to suspect that the true number of cases far outstripped the dozens reported and pressed Panjabi to move faster to expand testing, according to three people with knowledge of the conversations who were not authorized to comment.
U.S. officials on June 22 announced that they had lined up contracts with major lab companies such as Quest Diagnostics to perform monkeypox testing. But it would take several more weeks for thousands more testing locations to be fully deployed.
June 24: 245 confirmed U.S. infections
As Pride Month wound down — after a flurry of dance parties, parades and casual sex — thousands of gay men who had celebrated with friends began to find lesions across their bodies, including their rectums or genitals, or develop fevers and fatigue.
In Baltimore on June 25, Brian Thomas spotted what looked like two ingrown hairs on his butt. Two days later in New York, Gerald Febles found what looked like a mosquito bite on his hand. In the same neighborhood, Joshua Wright noticed a scabbed-over lesion in his groin.
But as they sought help, those men and others were often misdiagnosed — or were bounced between health providers.
Seeking a test June 30, Wright called the local health department, who said he would need a physician referral. He went to an urgent care clinic where he recalls the doctor suspecting monkeypox but said the clinic was testing only patients with two or more lesions. The doctor swabbed his lesion anyway and said she would follow up, but Wright did not hear back and called the health department again, which suggested going to an emergency room. He did, and recalled ER staff telling him they believed the lesion was an ingrown hair and to return if symptoms worsened because they could authorize only 20 tests a day — which Wright did a few days later, after more lesions appeared.
The 31-year-old would soon develop a sore in his urethra that caused him to scream in pain when he urinated. He had begged the ER for treatment, but no one informed him that TPoxx, an antiviral in ample supply in the national stockpile, was an option.
The crisis had become impossible for New York officials to ignore, prompting them to make their entire supply of 1,000 Jynneos doses immediately available for eligible men who were possibly exposed to monkeypox. Appointments were quickly snapped up, and photos spread on social media of gay men waiting in long lines. Biden administration officials privately chastised New York health officials for exhausting the city’s vaccine supply in four days.
But New York’s model inspired other cities to make their vaccines immediately available, too, putting pressure on the Biden administration to expedite even more doses. Federal officials June 28 said they would begin rushing tens of thousands of more vaccines to clinics nationwide.
In North Carolina, those doses couldn’t come soon enough, thought Kody Kinsley, the state’s first openly gay health secretary. With limited vaccine supplies prioritized for hot spots such as New York and D.C., North Carolina could not launch its own campaign — even as Kinsley felt compelled to warn gay men that they faced the highest risk of exposure to monkeypox.
And other problems persisted.
Kinsley was scrolling through his phone while visiting a friend in July when he noticed a man tweeting at him profanely and condemning the state’s response to the outbreak. The man tweeted about his struggles to get doctors to test him for monkeypox and how he had to pester public health officials before they authorized a test that turned up positive.
Kinsley called the man, telling him bluntly that “clearly what has happened is that providers are not reading our guidance, not paying attention and not on the same page,” according to a recording the patient provided to The Post.
July 26: 4,184 confirmed infections
After another month of climbing cases, the world’s top health watchdog declared monkeypox a global public health emergency on July 23, overruling the recommendation against doing so by an expert panel in hopes of pressuring governments into action.
In the United States, senior officials spent the weekend debating whether to declare their own health emergency, with Fauci, CDC Director Rochelle Walensky and other key leaders pushing for one. A public health emergency would unlock federal powers to compel health providers to report monkeypox data, tee up flexibility on vaccines and treatments, and raise awareness of the outbreak, they argued.
But the White House was navigating increasingly complicated domestic politics: Advocates had pressed the administration to declare emergencies for abortion, climate change and gun violence, key priorities for Democratic voters. Some administration officials wondered why the Biden administration needed a public health emergency for a virus seemingly contained among men who had sex with men, with no confirmed deaths and with existing treatments and vaccines.
As HHS Secretary Xavier Becerra and his deputies weighed a decision, White House Chief of Staff Ron Klain exhorted them to expedite vaccine doses that had been stuck in Denmark and treatments that were proving difficult to pry out of the national stockpile, three people with knowledge of the conversations said.
State health officials were privately warning that ordering vaccines from the stockpile relied on email and limited delivery to only five sites in each state. It caused confusion and “hours of additional work for already overburdened state and local public health staff,” according to a July 15 memo to the CDC from a group representing front-line immunization staff.
Publicly, key officials continued to insist the monkeypox outbreak response was going well.
On July 26, about 20 health officials and public health experts gathered at the Eisenhower Executive Office Building for an update on monkeypox led by Panjabi and O’Connell.
“It felt a bit they were trying to rehash all the things they had already done to try to reclaim some sense of success and readiness,” said Kinsley, the North Carolina health secretary, who attended the session. “They were trying really, really hard, for sure, but I think there’s a lot that was still missing.”
Tom Inglesby, director of the Johns Hopkins Center for Health Security, was the first to pose a question, asking whether the White House was still committed to ending the outbreak, or whether it was too late, according to several attendees.
Panjabi replied that “the only worthy goal is to contain” the virus — and eliminate it.
Inside the CDC emergency operations center in Atlanta that day, a wall of screens once dominated by coronavirus data now displayed graphs showing monkeypox infections soaring across the world and a global map with the United States in bright red.
Nine days later, on Aug. 4, the Biden administration declared a public health emergency.
Aug. 9: 9,492 confirmed U.S. infections
As the cameras switched on and a White House briefing began, the lights shone on two officials about to be introduced as the new leaders of America’s monkeypox response.
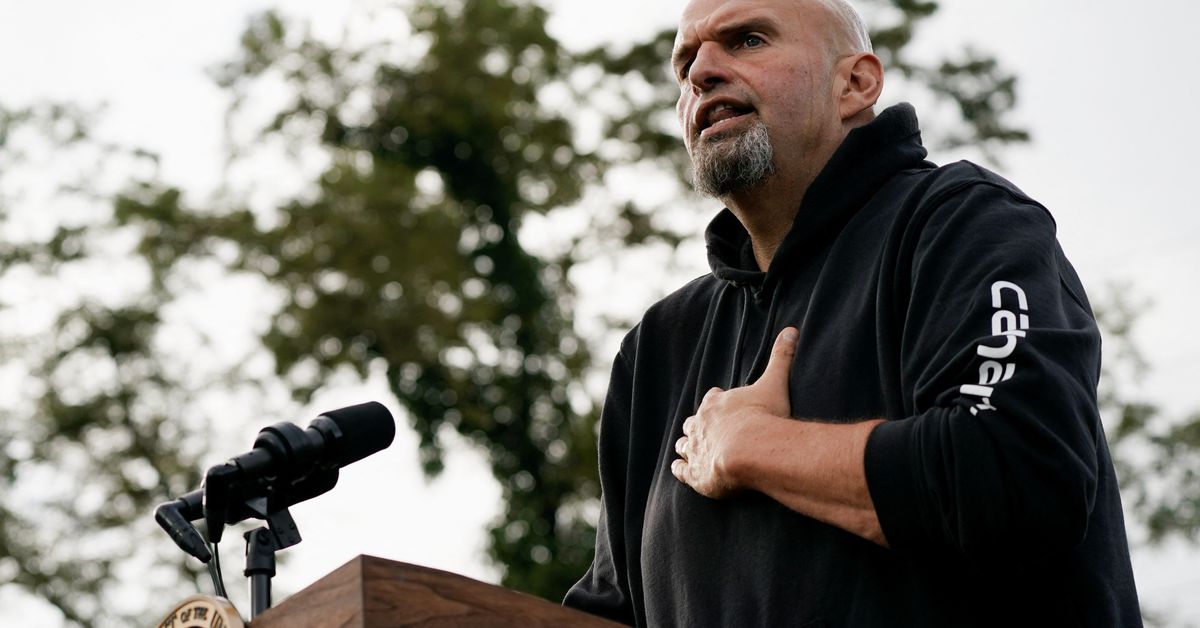
Fenton had won the White House’s trust for helping set up coronavirus vaccination centers in 2021. Now, the federal logistics expert was trying to draw on lessons from responding to the Sept. 11 terrorist attacks, Hurricane Katrina and other disasters.
The job today: Explain the nation’s plan to split vaccine doses in fifths and administer them with a new injection method, transforming about 441,000 doses of Jynneos into more than 2 million potential shots. The plan was finalized by the FDA over the pharmaceutical company’s safety concerns and after the company backed away from its CEO’s threat to cancel future orders.
The strategy is “a game changer when it comes to our response and our ability to get ahead of the virus,” the husky former college football player and longtime FEMA official told reporters.
Sitting next to Fenton was Daskalakis, his new top deputy. The CDC official had quickly become a White House favorite for his willingness to speak frankly to gay men about their risks — drawing on his experience not just as an infectious-disease physician but also as an openly gay man.
As the two men — whom some administration officials have affectionately nicknamed “the odd couple,” for their contrasting styles and approaches — led the briefing, other senior officials, including Becerra and Walensky, beamed in on Zoom screens behind them. The visual aimed to project a new narrative of the White House reasserting control over the monkeypox response.
The original face of the White House’s response, Panjabi, was nowhere to be seen. Watson, his spokeswoman, said the pandemic office leader had shifted back to broader priorities, a sign the “system is working as intended.”
September: To be determined
In New Orleans, Chuck Robinson, owner of Napoleon’s Itch gay bar on Bourbon Street, feels a sense of dread as the upcoming Southern Decadence festival draws closer and ominous headlines about monkeypox pop up on his phone.
The five-day celebration over Labor Day weekend likened to a gay Mardi Gras typically attracts tens of thousands. This year was supposed to be the grand return of the Bourbon Street Extravaganza, a free concert organized by Robinson and one of the festival’s largest events, after back-to-back pandemic cancellations. The time for a festival that has gone from reviled as moral affront to New Orleans to embraced by city leaders to come roaring back. But the new viral threat is spreading among gay men and through close contact — the kind rampant at his concert.
“They are neck to neck, and they are without their shirts, and they are sweating, and it will be hot, and my event will create that jampacked situation,” said Robinson, 81.
He scanned the news last week over morning coffee. An article on NOLA.com about the first mass monkeypox vaccination clinic at another gay bar said the line to get in stretched a block and a half; all shots were claimed within 30 minutes.
Robinson reached for a cigarette.
“I thought, ‘Oh, my God’ as I began to see the intensifying danger,” he said.
He’d already seen headlines out of Los Angeles, New York and Atlanta about chaos at vaccine sites — the uncertainty and fear resembling the early days of AIDS, he said.
He did the mental math. So many gay men across the country still struggling to get vaccinated. A second dose needed 28 days after the first shot. At least 14 days after the second dose for full protection. The festival just 24 days away.
It wasn’t enough time for those lining up now for shots, let alone those turned away, to be shielded before Southern Decadence.
Robinson and other organizers had fought for years to legitimize the festival: Would a superspreader event undermine all that?
His unease grew over the weekend as he watched monkeypox cases top 11,000.
He decided to call the party off.
[ad_2]
Source link