[ad_1]

- Vaginal health, including vaginal flora, is essential to well-being and fertility.
- The success rate of fertility treatments, such as IVF, can be affected by many factors including the composition of the vaginal microbiome prior to treatment.
- Recent findings suggest that probiotics administered vaginally for 10 days before fertility treatment may not improve unfavorable vaginal microbiomes.
The importance of probiotics and maintaining the “good” bacteria in the body is essential in many areas of health. The microorganisms that inhabit the vagina can impact pregnancy and other health outcomes.
However, improving the vaginal microbiome might not be as simple as taking probiotics. Experts shared recent study findings at the 38th annual meeting of the European Society of Human Reproduction and Embryology (ESHRE).
They found that treatment with vaginal probiotic capsules among women with unfavorable vaginal microbiomes did not improve vaginal flora more than a placebo.
The
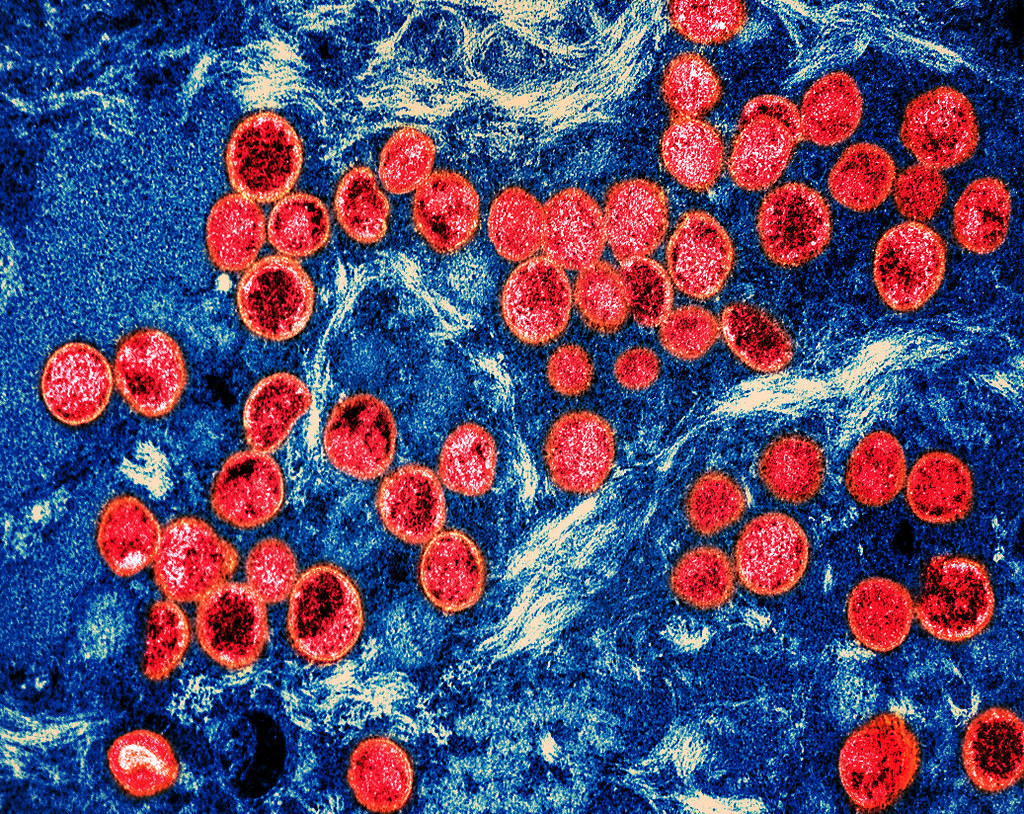
People’s microbiomes play a crucial role in many areas of health. The vaginal microbiome refers to all the microorganisms in the vagina. The
It can also impact the risk for sexually transmitted infections. Finally, it can also affect
Doctors must consider vaginal health and how to improve it, including for those seeking infertility treatment such as in vitro fertilization (IVF).
A healthy vaginal microbiome can increase the chances of a healthy pregnancy. However, how to best improve vaginal microbiomes might be more complicated than just using vaginal probiotics.
The study in question was a randomized, double-blind, placebo-controlled study, which allows for great objectivity and helps remove the risk of bias. Researchers included 74 participants. The participants had all been referred for IVF and had unfavorable vaginal microbiomes.
Researchers divided the participants into two groups: One received a placebo, and the other received vaginal probiotic capsules that contained Lactobacillus. The researchers reevaluated the participants’ vaginal microbiomes after they had completed their treatment and after they had had their next menstrual cycle.
The study authors found no significant differences between the control and intervention groups. However, more than a third (34.2%) of all participants experienced improvements in vaginal microbiome quality over 1-3 months, regardless of whether they received a probiotic or a placebo.
Yasser Diab, consultant gynecologist and obstetrician at the Cadogan Clinic, who was not involved in this study, noted to Medical News Today that “[t]here was no significant difference between the two groups — the lactobacilli group [and the] placebo group.”
“The intervention did not include all strains of lactobacilli implicated in influencing fertility outcomes. More detailed studies are needed to establish therapeutic strategies to improve fertility treatment outcomes from interventions addressing the vaginal microbiome,” he pointed out.
Study author Dr. Ida Enberg Jepson commented that she and her colleagues were surprised by the results and that specific probiotic treatments might not be as effective as they had hoped.
She explained for MNT:
“The study indicates that the ‘rush to probiotics’ should be cautiously tempered. We found that the use of a specific probiotic containing Lactobacillus rhamnosus and Lactobacillus gasseri did not improve an (asymptomatic) unfavorable vaginal microbiota in infertile women.”
When sharing the study’s findings, its authors noted a few limitations. First of all, the vaginal probiotic capsules did not contain all the strains of Lactobacilli that may influence fertility outcomes. They also noted that their broad categorization of low, medium, and high vaginal microbiome profiles may have masked subtle changes.
The study does not negate the importance of vaginal health. However, it does open up questions about how to best address vaginal health, particularly when working toward optimal vaginal microbiomes before infertility treatments.
Dr. Jepson further noted a few areas for potential further research:
“Suggestions for new research could be exploring different Lactobacilli strains or investigating vaginal microbiota transplantation from women with normal vaginal microbiota. Furthermore, it would be interesting to investigate if it is possible to achieve a higher pregnancy rate if we postpone IVF treatment in patients with an unfavorable vaginal microbiota until a spontaneous improvement is seen during the next 1–3 months, as this study suggests.”
Results may further influence future recommendations prior to IVF. Dr. Jepson explained that “[w]e saw a spontaneous improvement in the patients with an unfavorable vaginal microbiota, primarily with a low profile, over 1–3 months. This suggests that an idea for patients with an unfavorable vaginal microbiota could be to postpone IVF treatment until spontaneous improvement.”
[ad_2]
Source link